
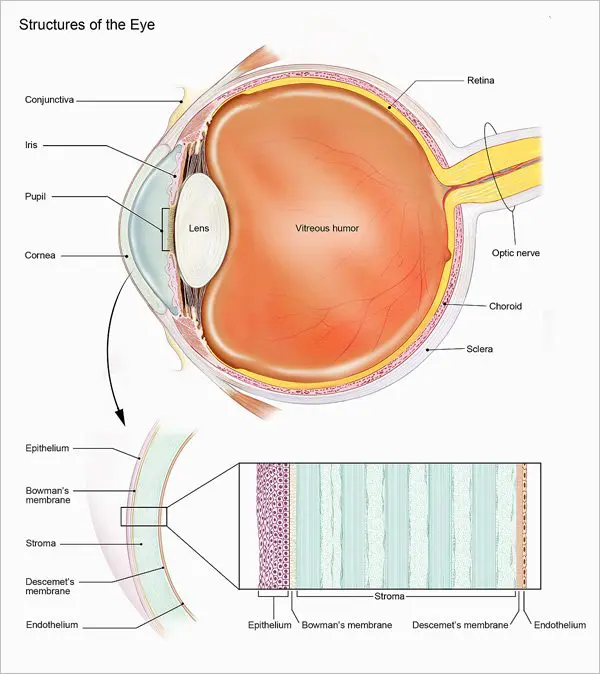
Cornea
The cornea is the eye’s outermost layer. It is the clear, domeshaped surface that covers the front of the eye. It plays an important role in focusing your vision.
Book a consultation

Although the cornea may look clear and seem to lack substance, it is a highly organised tissue. Unlike most tissues in the body, the cornea of eye contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from tears and the aqueous humor (a fluid in the front part of the eye that lies behind the cornea).
The tissues of the cornea are arranged in three basic layers, with two thinner layers, or membranes, between them. Each of these five layers has an important function. These layers are:
Epithelium
The epithelium is the cornea’s outermost layer. Its primary functions are to:
The corneal epithelium is filled with thousands of tiny nerve endings, which is why your eye may hurt when it is rubbed or scratched. The part of the epithelium that epithelial cells anchor and organize themselves to is called the basement membrane.
Bowman’s membrane
The next layer behind the basement membrane of the corneal epithelium is a transparent film of tissue called Bowman’s layer, composed of protein fibers called collagen. If injured, Bowman’s layer can form a scar as it heals. If these scars are large and centrally located, they may cause vision loss.
Stroma
Behind Bowman’s layer is the corneal stroma, which is the thickest layer of the cornea. The corneal stroma is composed primarily of water and collagen. Collagen gives the cornea its strength, elasticity, and form. The unique shape, arrangement, and spacing of collagen proteins are essential in producing the cornea’s light-conducting transparency.
Descemet’s Membrane
Behind the corneal stroma is Descemet’s membrane, a thin but strong film of tissue that serves as a protective barrier against infection and injuries. Descemet’s membrane is composed of collagen fibers that are different from those of the stroma, and are made by cells in the endothelial layer of the cornea (see above). Descemet’s membrane repairs itself easily after injury.
Endothelium
The endothelium is the thin, innermost layer of the cornea. Endothelial cells are important in keeping the cornea clear. Normally, fluid leaks slowly from inside the eye into the stroma. The endothelium’s primary task is to pump this excess fluid out of the stroma. Without this pumping action, the stroma would swell with water and become thick and opaque.
In a healthy eye, a perfect balance is maintained between the fluid moving into the cornea and the fluid pumping out of the cornea. Unlike the cells in Descemet’s membrane, endothelial cells that have been destroyed by disease or trauma are not repaired or replaced by the body.
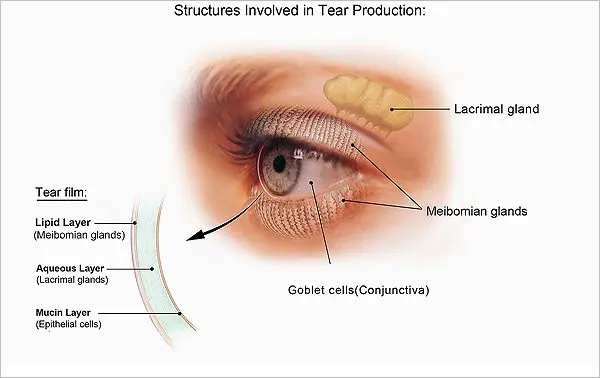
Every time we blink, tears are distributed across the cornea to keep the eye moist, help wounds heal, and protect against infection. Tears form in three layers:
The cornea acts as a barrier against dirt, germs, and other particles that can harm the eye. The cornea shares this protective task with the eyelids and eye sockets, tears, and the sclera (white part of the eye). The cornea also plays a key role in vision by helping focus the light that comes into the eye. The cornea is responsible for 65-75 percent of the eye’s total focusing power.
The cornea and lens of the eye are built to focus light on the retina, which is the light-sensitive tissue at the back of the eye. When light strikes the cornea, it bends—or refracts—the incoming light onto the lens. The lens refocuses that light onto the retina, which starts the translation of light into vision. The retina converts light into electrical impulses that travel through the optic nerve to the brain, which interprets them as images.
The refractive process the eye uses is similar to the way a camera takes a picture. The cornea and lens in the eye act as the camera lens. The retina is like the film (in older cameras), or the image sensor (in digital cameras). If the image is not focused properly, the retina makes a blurry image.
The cornea also serves as a filter that screens out damaging ultraviolet (UV) light from the sun. Without this protection, the lens and the retina would be exposed to injury from UV rays.
Injuries
After minor injuries or scratches, the cornea usually heals on its own. Deeper injuries can cause corneal scarring, resulting in a haze on the cornea that impairs vision. If you have a deep injury, or a corneal disease or disorder, you could experience:
If you experience any of these symptoms, seek help from an eye care professional.
Allergies
The most common corneal disorders from allergies that affect the eye are those related to pollen, particularly when the weather is warm and dry. Symptoms in the eye include redness, itching, tearing, burning, stinging, and watery discharge, although usually not severe enough to require medical attention. Antihistamine decongestant eyedrops effectively reduce these symptoms. Rain and cooler weather, which decreases the amount of pollen in the air, can also provide relief. For more information see Facts about Pink Eye (Conjunctivitis).
Keratitis
Keratitis is a common corneal disorder due to inflammation of the cornea. Noninfectious keratitis is a corneal condition that can be caused by a minor injury, or from wearing contact lenses too long. Infection is the most common cause of keratitis. Infectious keratitis can be caused by bacteria, viruses, fungi or parasites. Often, these infections are also related to contact lens wear, especially improper cleaning of contact lenses or overuse of old contact lenses that should be discarded. Minor corneal infections are usually treated with antibacterial eye drops. If the problem is severe, it may require more intensive antibiotic or antifungal treatment to eliminate the infection, as well as steroid eye drops to reduce inflammation.
Dry eye
Dry eye is a condition in which the eye produces fewer or lower quality tears and is unable to keep its surface lubricated due to this lack of tear fluid.
The main symptom of dry eye is usually a scratchy feeling or as if something is in your eye. Other symptoms include stinging or burning in the eye, episodes of excess tearing that follow periods of dryness, discharge from the eye, and pain and redness in the eye.
Sometimes people with dry eye also feel as if their eyelids are very heavy or their vision is blurred.
A corneal dystrophy is a condition in which one or more parts of the cornea lose their normal clarity due to a buildup of material that clouds the cornea. These corneal dystrophies:
Corneal dystrophies affect vision in different ways. Some corneal dystrophies severe visual impairment, while a few corneal dystrophies cause no vision problems and are only discovered during a routine eye exam. Other dystrophies may cause repeated episodes of pain without leading to permanent vision loss. Some of the most common corneal dystrophies include keratoconus, Fuchs’ dystrophy, lattice dystrophy, and map-dot-fingerprint dystrophy.
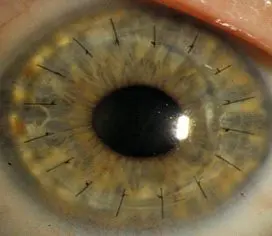
Keratoconus
Kerataconus is a progressive thinning of the cornea. It is the most common corneal dystrophy in the U.S., affecting one in every 2,000 Americans. It is most prevalent in teenagers and adults in their 20s.
Keratoconus causes the middle of the cornea to thin, bulge outward, and form a rounded cone shape. This abnormal curvature of the cornea can cause double or blurred vision, nearsightedness, astigmatism, and increased sensitivity to light.
The causes of keratoconus aren’t known, but research indicates it is most likely caused by a combination of genetic susceptibility along with environmental and hormonal influences. About 7 percent of those with the condition have a history of kerataconus in their family. Keratoconus is diagnosed with a slit-lamp exam. Your eye care professional will also measure the curvature of your cornea.
Keratoconus usually affects both eyes. At first, the condition is corrected with glasses or soft contact lenses. As the disease progresses, you may need specially fitted contact lenses to correct the distortion of the cornea and provide better vision.
In most cases, the cornea stabilizes after a few years without causing severe vision problems. A small number of people with keratoconus may develop severe corneal scarring or become unable to tolerate a contact lens. For these people, a corneal transplant may become necessary.
Fuchs’ Dystrophy
Fuchs’ dystrophy is a slowly progressing corneal disease that usually affects both eyes and is slightly more common in women than in men. It can cause your vision to gradually worsen over many years, but most people with Fuchs’ dystrophy won’t notice vision problems until they reach their 50s or 60s.
Fuchs’ dystrophy corneal disease s caused by the gradual deterioration of cells in the corneal endothelium; the causes aren’t well understood. Normally, these endothelial cells maintain a healthy balance of fluids within the cornea. Healthy endothelial cells prevent the cornea from swelling and keep the cornea clear. In Fuchs’ dystrophy, the endothelial cells slowly die off and cause fluid buildup and swelling within the cornea. The cornea thickens and vision becomes blurred.
As the disease progresses, Fuchs’ dystrophy symptoms usually affect both eyes and include:
The first step in treating Fuchs’ dystrophy is to reduce the swelling with drops, ointments, or soft contact lenses. If you have severe disease, your eye care professional may suggest a corneal transplant.
Lattice Dystrophy
Lattice dystrophy gets its name from a characteristic lattice-like pattern of deposits in the stroma layer of the cornea. The deposits are made of amyloid, an abnormal protein fiber. Over time, the deposits increase and the lattice lines grow opaque, take over more of the stroma, and gradually converge to impair vision.
Although lattice dystrophy can occur at any time in life, it most commonly begins in childhood between the ages of 2 and 7. In some people, amyloid deposits can accumulate under the epithelium of the cornea. This can erode the epithelium, and cause a condition known as recurrent epithelial erosion. This erosion alters the cornea’s normal curvature and causes temporary vision problems. It can also expose the nerves that line the cornea and cause severe pain.
To ease this pain, an eye care professional may prescribe eye drops and ointments to reduce the friction of the eyelid against the cornea. In some cases, an eye patch may be used to immobilize the eyelid. The erosions usually heal within days, although you may have some pain for the next six to eight weeks.
By age 40, some people with lattice dystrophy have scarring under the epithelium that can impact vision to such an extent that the most effective treatment will be a corneal transplant. Although the early results of corneal transplantation are typically good, lattice dystrophy may reappear later and require long-term treatment.
Map-Dot-Fingerprint Dystrophy
Map-Dot-Fingerprint dystrophy, also known as epithelial basement membrane dystrophy, occurs when the basement membrane develops abnormally and forms folds in the tissue. The folds create gray shapes that look like continents on a map. There also may be clusters of opaque dots underneath or close to the maplike patches. Less frequently, the folds form concentric lines in the central cornea that resemble small fingerprints.
Symptoms of htis corneal disease blurred vision, pain in the morning that lessens during the day, sensitivity to light, excessive tearing, and a feeling that there’s something in the eye.
Map-dot-fingerprint dystrophy usually occurs in both eyes and affects adults between the ages of 40 and 70, although it can develop earlier in life. Typically, map-dot-fingerprint dystrophy will flare up now and then over the course of several years and then go away, without vision loss. Some people can have map-dot-fingerprint dystrophy but not experience any symptoms.
Others with the disease will develop recurring epithelial erosions, in which the epithelium’s outermost layer rises slightly, exposing a small gap between the outermost layer and the rest of the cornea. These erosions alter the cornea’s normal curvature and cause blurred vision. They may also expose the nerve endings that line the tissue, resulting in moderate to severe pain over several days.
The discomfort of epithelial erosions can be managed with topical lubricating eye drops and ointments. If drops or ointments don’t relieve the pain and discomfort, there are outpatient surgeries including:
Herpes Zoster (Shingles)
Shingles is a reactivation of the varicel-lazoster virus, the same virus that causes chickenpox. If you have had chickenpox, the virus can live on within your nerve cells for years after the sores have gone away. In some people, the varicel-lazoster virus reactivates later in life, travels through the nerve fibers, and emerges in the cornea. If this happens, your eye care professional may prescribe oral anti-viral treatment to reduce the risk of inflammation and scarring in the cornea. Shingles can also cause decreased sensitivity in the cornea.
Corneal problems may arise months after the shingles are gone from the rest of the body. If you experience shingles in your eye, or nose, or on your face, it’s important to have your eyes examined several months after the shingles have cleared.
Ocular Herpes
Herpes of the eye, or ocular herpes, is a recurrent viral infection that is caused by the herpes simplex virus (HSV-1). This is the same virus that causes cold sores. Ocular herpes can also be caused by the sexually transmitted herpes simplex virus (HSV-2) that causes genital herpes.
Ocular herpes can produce sores on the eyelid or surface of the cornea and over time the inflammation may spread deeper into the cornea and eye, and develop into a more severe infection called stromal keratitis. There is no cure for ocular herpes, but it can be controlled with antiviral drugs.
Iridocorneal Endothelial Syndrome (ICE)
Iridocorneal endothelial syndrome (ICE) is more common in women and usually develops between ages 30-50. ICE has three main features:
ICE is usually present in only one eye. It is caused by the movement of endothelial cells from the cornea to the iris. This loss of cells from the cornea leads to corneal swelling and distortion of the iris and pupil. This cell movement also blocks the fluid outflow channels of the eye, which causes glaucoma.
There is no treatment to stop the progression of ICE, but the glaucoma is treatable. If the cornea becomes so swollen that vision is significantly impaired, a corneal transplant may be necessary.
Pterygium
A pterygium is a pinkish, triangular tissue growth on the cornea. Some pterygia (plural for pyterygium) grow slowly throughout a lifetime, while others stop growing. A pterygium rarely grows so large that it covers the pupil of the eye.
Pterygia are more common in sunny climates and in adults 20-40 years of age. It’s unclear what causes pterygia. However, since people who develop pterygia usually have spent significant time outdoors, researchers believe chronic exposure to UV light from the sun may be a factor.
To protect yourself from developing pterygia, wear sunglasses, or a wide-brimmed hat in places where the sunlight is strong. If you have one or more pterygia, lubricating eye drops may be recommended to reduce redness and soothe irritation.
Because a pterygium is visible, some people might want to have it removed for cosmetic reasons. However, unless it affects vision, surgery to remove a pterygium is not recommended. Even if it is surgically removed, a pterygium may grow back, particularly if removed before age 40.
Stevens Johnson Syndrome
Stevens-Johnson Syndrome (SJS), also called erythema multiforme major, is a disorder of the skin that also affects the eyes. SJS is characterized by painful blisters on the skin and the mucous membranes of the mouth, throat, genitals, and eyelids.
Often, SJS begins with flu-like symptoms, followed by a painful red or purplish rash of blisters that spread. SJS can cause severe conjunctivitis, iritis (an inflammation inside the eye), corneal blisters and erosions, and corneal holes. In some cases, SJS can lead to significant vision loss.
The most commonly cited cause of SJS is an allergic reaction to a drug or medication, particularly sulfa drugs. It is also associated with viral infections.
Treatment for the eye may include artificial tears or lubricating eye drops, antibiotics, or corticosteroids. About one third of those who develop SJS will have one or more episodes of the disease. SJS occurs twice as often in men as in women, and most often affects children and young adults under 30, although it can develop at any age.
PTK
Phototherapeutic keratectomy (PTK) is a surgical technique that uses UV light and laser technology to reshape and restore the cornea for patients. PTK has been used to treat recurrent erosions and corneal dystrophies, such as map-dot-fingerprint dystrophy and basal membrane dystrophy. PTK helps delay or postpone corneal grafting or replacement.
Corneal Transplant Surgery
Corneal transplant surgery removes the damaged portion of the cornea from patients and replaces it with healthy donor tissue. Corneas are the most commonly transplanted tissue worldwide. More than 47,000 corneal transplants were performed in the U.S. in 2014.
In the past, the standard approach to corneal transplants was to surgically replace the entire cornea with donor tissue, a technique known as penetrating keratoplasty. This is called a full thickness transplant, and may still be the only option for people with advanced keratoconus and scarring, severe herpetic scarring, or traumatic injury that affects the whole cornea.
However, most people who need corneal transplantation undergo a newer procedure called lamellar keratoplasty. This is called a partial thickness transplant. In this procedure, the surgeon selectively removes and replaces the diseased layer(s) of the cornea and leaves the healthy tissue in place. Replacing only diseased layers with a donor graft leaves the cornea more structurally intact and leads to a lower rate of complications and better visual improvement.
Anterior lamellar keratoplasty removes damaged stromal tissue and replaces it with healthy stroma from a donor. This procedure is used for:
Endothelial lamellar keratoplasty removes diseased endothelial tissue and replaces it with healthy endothelium from a donor. This procedure is used for:
Corneal transplants are generally done under local anesthetic as an outpatient procedure. With full thickness transplants, the damaged cornea is removed and replaced with a donor cornea. Tiny stitches secure the transplant. Partial thickness transplants use fewer stitches. Either type of surgery usually takes 30 minutes.
Artificial Cornea
A keratoprosthesis (KPro) is an artificial cornea. A KPro may be the only option available for people who have not had success with corneal tissue implants or who have a high risk of tissue rejection (such as those with Stevens-Johnson syndrome or severe chemical burns).
The Boston type-1 KPro is the most used keratoprosthesis. It is made of clear plastic and consists of three parts, with donor cornea tissue clamped between front and back plates. When fully assembled it has the shape of a collar button. The procedure to insert a KPro is performed by an ophthalmologist, usually on an outpatient basis.
Improved corneal wound healing could have an impact on many types of disorders and injuries of the cornea. NEI researchers are conducting trials and studies to better understand how the cornea naturally heals after injury, which involves the release of proteins that act together to move the epithelial layer over the wound. This research could lead to new therapeutic strategies for transplantation and other treatments to repair corneal damage.
Other research seeks to improve the success of corneal grafts. For example, one study is looking at immune system factors that influence whether or not a graft will integrate and attach successfully. Identifying these factors could lead to new ways to promote graft survival without the use of strong immunosuppressive medications that can put people at risk for infections.
There is an increasing need for development and refinement of artificial (prosthetic) corneas. The demand for human corneal tissue is growing, but the supply is falling due to the popularity of LASIK surgeries, which weaken the corneal stroma and make it unsuitable for donation.
The development of endothelial stem cell lines is an area of research being explored by a number of NEI-supported investigators. The goal of this research is to create stem cells that can be used as a laboratory model to test potential therapies, or used as therapies on their own to promote regrowth of healthy corneal tissue. For example, one group of researchers is developing a source of human corneal endothelial stem cells, and a procedure to implant them into the eye and restore clear vision.
Research to improve the diagnosis of corneal diseases and disorders is another priority for NEI. For example, keratoconus is the most common degenerative disease affecting the cornea. In its earliest stages, kerataconus is difficult to detect and may go untreated.
Fuchs’ dystrophy accounts for most of the corneal transplants performed each year in the U.S. To identify new treatment approaches, NEI-supported researchers are searching for genetic mutations that are associated with Fuchs’ dystrophy. Such genes could be targets for future therapies.
Herpetic stromal keratitis caused by herpes simplex virus (HSV) infection is the most common cause of corneal blindness in the developed world. One group of researchers is developing a vaccine that, if successful, will lead to a significant reduction in the transmission of HSV to the cornea.
NEI is supporting a number of clinical trials in the U.S. to confirm that corneal collagen cross-linking (CXL) is safe and effective. CXL is a minimally-invasive surgical procedure that combines a photosensitive solution applied to the cornea with a low dose of UV light. The photosensitive solution reacts with the UV light to create new collagen bonds (cross-links) that strengthen the cornea. CXL has been approved in Europe and Canada for treating kerataconus.
Last Reviewed: May 2016
Courtesy: The National Eye Institute (NEI) is part of the National Institutes of Health (NIH) and is the Federal government’s lead agency for vision research that leads to sight-saving treatments and plays a key role in reducing visual impairment and blindness.
Request a Brochure
