- Lens Surgery

Cataract Surgery

- Treatment

- Lens Surgery
Cataract Surgery
Cataract surgery is one of the oldest forms of surgery recorded. Technological advances have turned cataract laser surgery into one of the safest and most regularly performed procedures for adults worldwide.
What is Cataract Surgery?
Cataract surgery involves the removal of the cloudy natural lens of the eye (the cataract) and replacing it with a carefully selected intraocular lens (IOL).
There are several designs of intraocular lenses (IOLs) available, each having their own strengths in performance. The choice of lens has a major influence on the outcome of cataract extraction surgery and whether glasses would be required afterwards. Whilst the NHS offers an excellent service for cataract surgery, there is rarely an option for choosing your intraocular lens, meaning that glasses will almost certainly be required.
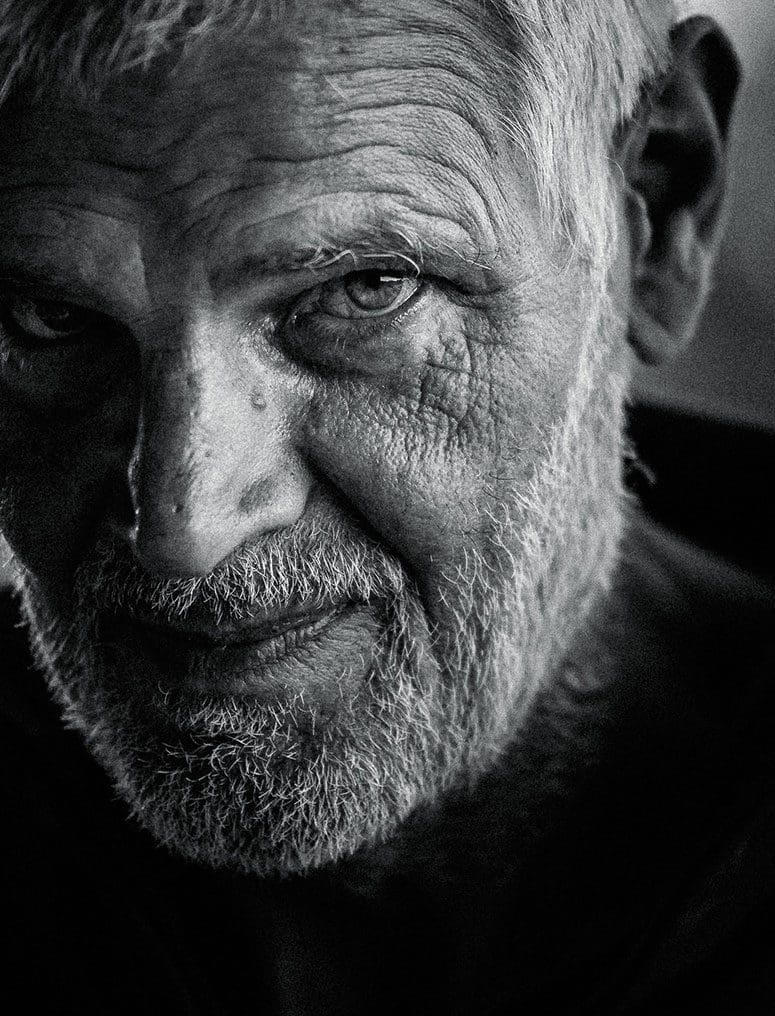
Leading Cataract Surgeons
All our UK cataract surgeons specialise in cataract surgery and have all performed several thousand cataract procedures on adults in the UK, particularly for patients with high spectacle corrections, complex cataracts and following other types of refractive surgery.
Today, thanks to advances in technology, most patients experience little or no pain and return to their normal activities the day after eye surgery
The decision to undergo cataract surgery offers a once-in-a-lifetime opportunity to insert the best lens for you.

With modern surgical techniques it is possible for an eye surgeon to operate on a cataract at a relatively early stage, contrary to the misconception of the cataract needing to be mature or ‘ripe’.
There is no specific level of vision at which cataract removal surgery is indicated; but it is usually recommended if your quality of life is significantly impacted. Surgery is also indicated if you wish to drive and your vision no longer meets the necessary DVLA legal standard.
With modern surgical techniques it is possible for an eye surgeon to operate on a cataract at a relatively early stage, contrary to the misconception of the cataract needing to be mature or ‘ripe’.
There is no specific level of vision at which cataract removal surgery is indicated; but it is usually recommended if your quality of life is significantly impacted. Surgery is also indicated if you wish to drive and your vision no longer meets the necessary DVLA legal standard.


How is it performed?
- 1.Local anaesthetic eye drops are applied to both eyes
- 2.The area around your eye will be washed and cleansed and a sterile drape will be applied
- 3.An instrument is gently positioned to hold your eyelids open
- 4.Your eye doctor will use ultrasound energy to liquefy the lens which can then be aspirated
- 5.A new lens will be inserted using an injection system
- 6.The lens is unfolded and positioned within the eye